The factors that cause patellofemoral pain are complex, and researches are currently not completely clear. However, several theoretical models have been described. These include altered patellar tracking, resulting in elevated patellofemoral joint contact pressure, and a loss of tissue homeostasis in the surrounding innervated tissues including the synovial lining or fat pad, among others.
In this section, you will find information about the proposed theories linked to the aetiology of patellofemoral pain.
 Altered movements are thought to overload the knee joint during functional activities (e.g. climbing stairs, squatting, running) leading to patellar maltracking. This maltracking subsequently increases patellofemoral joint stress, initiating nociceptive firing from the densely innervated subchondral bone.
Altered movements are thought to overload the knee joint during functional activities (e.g. climbing stairs, squatting, running) leading to patellar maltracking. This maltracking subsequently increases patellofemoral joint stress, initiating nociceptive firing from the densely innervated subchondral bone.
1 – Pelvis drops on opposite side, placing increased tension on the outside of the leg and pulling the knee cap outward.
2 – Hip collapses inward and rolls under the knee cap due to poor function and weakness of the hip muscles.
3 – Thigh muscles are weak or function poorly, meaning there is inadequate support for the knee and knee cap.
4- Foot rolls in too much, causing the shin and knee to collapse inward under the knee cap.
The presentation of biomechanical deficits in patients with patellofemoral pain is both common and varied. Therefore, clinicians should carefully assess the movement patterns throughout the kinetic chain during different tasks, as identified biomechanical deficits may indicate a more severe condition and can help guide an individual specific treatment plan.
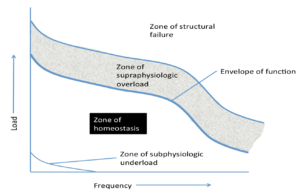 In the tissue homeostasis model Scott Dye describes how doing “too much” (supraphysiological over load) or “too little” (subphysiologic under load) may result in patellofemoral pain.
In the tissue homeostasis model Scott Dye describes how doing “too much” (supraphysiological over load) or “too little” (subphysiologic under load) may result in patellofemoral pain.
A resultant single loading event of sufficient magnitude or a number of repeated loading events of lower magnitude may result in the loss of tissue homeostasis, at least temporarily, and subsequent increase in nociceptive firing.
If patients do ‘too much too soon’ they will be at greater risk of developing or irritating knee pain.
Also, it is not good to do little or no exercise as their capacity for exercise and function will reduce.
If they progress their physical activities slowly (e.g. 10% per week) they will be less likely to develop or aggravate knee pain.
 The biomedical model in isolation possesses inherent limitations within the complex paradigm of human pain perception.
The biomedical model in isolation possesses inherent limitations within the complex paradigm of human pain perception.
Elevated levels of anxiety, depression, pain catastrophising and fear of movement have been reported in patients with patellofemoral pain, which have the capacity to negatively influence pain, physical function and activity related behaviours.
These observations, in combination with reductions in pain and disability being associated with improvements in psychosocial health, highlight the importance of recognising alterations in a patient’s pain processing during clinical examination and integrating these findings into their eventual management plan. It is also important to state that evidence does not currently support the notion that psychosocial factors are a primary driver of symptoms, instead evidence supports psychosocial factors are altered in those who already have patellofemoral pain.
PODCAST
SHORT INTERVIEW
Section under development: Here you will find a podcast or a short interview.


